What is Artificial Intelligence (AI) in Radiology? A Foundational Guide
Artificial Intelligence (AI) is one of the most transformative technologies of our time, and it is rapidly making its way into the field of medical imaging. In radiology, AI refers to the use of computer algorithms that can perform tasks that typically require human intelligence, such as interpreting medical images. These tools are not designed to replace human experts, but to augment and assist them, helping to improve efficiency, accuracy, and patient outcomes.
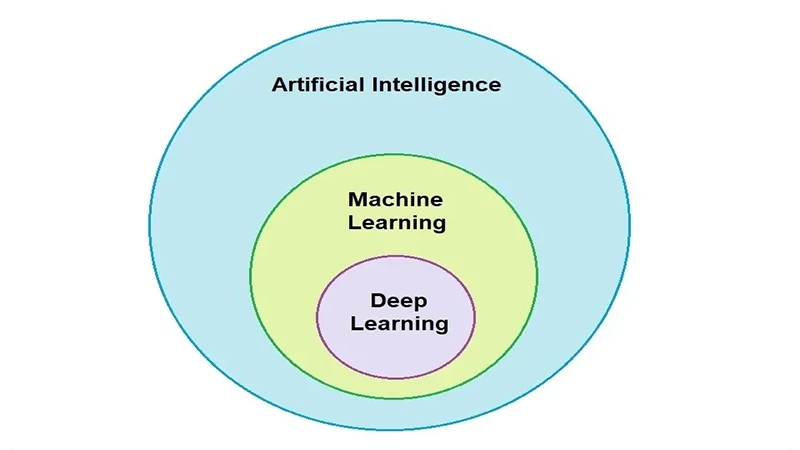
From Machine Learning to Deep Learning
The term "AI" is broad. Most AI in radiology today is a specific type called **Machine Learning**, and more specifically, **Deep Learning**.
- Machine Learning: This is a type of AI where a computer learns to identify patterns in data without being explicitly programmed. For example, developers might show an algorithm thousands of images of lung nodules and healthy lungs, and the algorithm learns the features that distinguish one from the other.
- Deep Learning: This is a more advanced subset of machine learning that uses complex, multi-layered "neural networks" inspired by the human brain. Deep learning algorithms can learn from vast amounts of data and can often identify incredibly subtle patterns that are not apparent to the human eye. Most cutting-edge radiology AI uses deep learning.
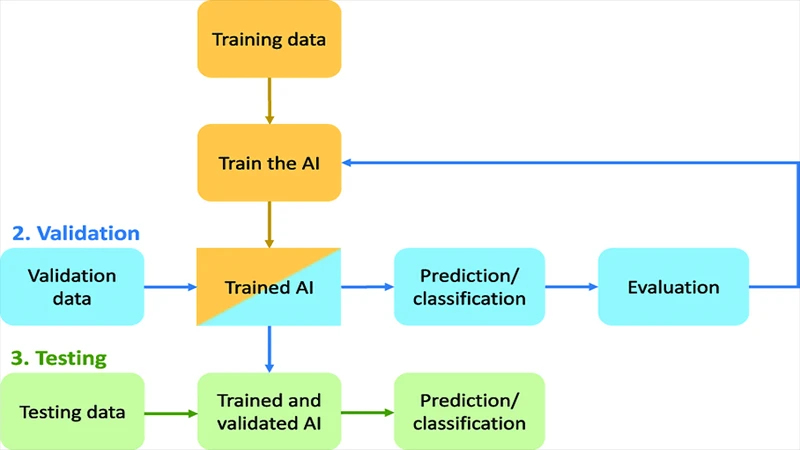
How Does a Radiology AI Get "Trained"?
An AI model doesn't start out smart. It has to be trained, much like a radiology resident. The training process involves several key steps:
- Data Collection: A huge, curated dataset of medical images is collected. For an AI that detects fractures, this would be thousands of X-rays.
- Annotation: Human experts (radiologists) must meticulously label these images. They draw boxes around every fracture, effectively teaching the algorithm "this is what a fracture looks like." This annotated data is the "ground truth."
- Training: The annotated dataset is fed into the deep learning model. The algorithm analyzes the images, makes a prediction (e.g., "fracture" or "no fracture"), and compares its answer to the ground truth.
- Learning: If the algorithm is wrong, it adjusts its internal parameters and tries again. This process is repeated millions of times, with the algorithm gradually getting better and better at recognizing the correct patterns.
- Validation & Testing: Finally, the trained model is tested on a completely new set of images it has never seen before to evaluate its real-world performance.
What Can AI Do in Radiology Today?
AI is not a single tool, but a collection of specialized applications. Current AI tools are being developed for a wide range of tasks:
- Detection: Identifying and highlighting potential abnormalities, such as a small lung nodule on a CT scan or a subtle fracture on an X-ray.
- Triage: Automatically flagging critical studies (like a brain bleed) and moving them to the top of a radiologist's worklist for immediate review.
- Quantification: Automatically measuring the size of a tumor or the volume of an organ, tasks that can be tedious and time-consuming for humans.
- Workflow Improvement: Automating protocoling of scans and improving technologist workflow.
Conclusion: An Assistant, Not a Replacement
The goal of AI in radiology is to create a powerful partnership between human intelligence and machine precision. AI excels at repetitive, data-intensive tasks, freeing up radiologists and technologists to focus on complex problem-solving, patient interaction, and the holistic interpretation of medical findings. By handling the tedious work and providing a "second set of eyes," AI has the potential to make the field of medical imaging more accurate, efficient, and ultimately, more valuable for patient care.


Comments